Risk factors
The exact cause of ulcerative colitis is unknown. Risk factors may include:
Age
Ulcerative colitis usually begins before the age of 30. But, it can occur at any age.
Race or ethnicity
Although whites have the highest risk of the disease, it can occur in any race.
Family history
You’re at higher risk if you have a close relative, such as a parent, sibling or child, with the disease.
Environment factors
Nonsteroidal anti-inflammatory drugs, antibiotics, and oral contraceptives may slightly increase the chance of developing ulcerative colitis. A high-fat diet may also slightly increase the chance of getting ulcerative colitis.
Diagnosis
Routine Blood tests
Your doctor may suggest blood tests to check for anemia — a condition in which there aren’t enough red blood cells to carry adequate oxygen to your tissues — or to check for signs of infection.
Fecal Blood Test
White blood cells in your stool can indicate ulcerative colitis. A stool sample can be checked for signs of infection, as gastroenteritis which sometimes have similar symptoms to ulcerative colitis.
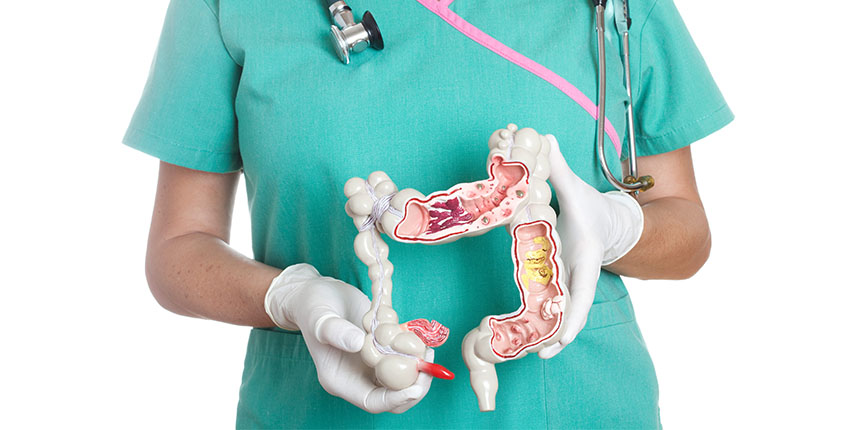
Colonoscopy
A colonoscopy uses a flexible tube containing a camera called a colonoscope, which allows your entire colon to be examined. A biopsy sample can also be taken.
Sigmoidoscopy
During this procedure, only the rectum and lower part of the colon are examined. A biopsy sample can also be taken.
X-ray
If you have severe symptoms, your doctor may use a standard X-ray of your abdominal area to rule out serious complications, such as a perforated colon.
CT scan
A CT scan of your abdomen or pelvis may be performed if your doctor suspects a complication from ulcerative colitis or inflammation of the small intestine. A CT scan may also reveal how much of the colon is inflamed
MRI
MRI is very helpful in diagnosing and managing ulcerative colitis.
Lifestyle and home remedies
Problems such as diarrhea, abdominal pain and gas improve by limiting or eliminating dairy products.
Fat passes through your intestine, making your diarrhea worse. Try low-fat foods.
High-fiber foods, such as fresh fruits and vegetables and whole grains, may make your symptoms worse.
Spicy foods, alcohol and caffeine may make your signs and symptoms worse.
Eat small meals. You may find you feel better eating five or six small meals a day rather than two or three larger ones.
Drink plenty of liquids. Try to drink plenty of fluids daily. Water is best.
Multivitamin and mineral supplements are often helpful.
Even mild exercise can help reduce stress, relieve depression and normalize bowel function.
Biofeedback (stress-reduction technique) helps you reduce muscle tension and slow your heart rate with the help of a feedback machine.
Regular relaxation and breathing exercises like yoga and meditation are effective ways to cope with stress.
References:
http://www.nhs.uk/Conditions/Ulcerative-colitis/Pages/Diagnosis.aspx
http://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/basics/risk-factors/con-20043763