Faecal Occult Blood Testing (60 – 69 years)
All men and women aged 60-69 will be offered a Faecal Occult Blood Test (FOBT) every two years. The symptoms of bowel cancer vary and not everybody will have symptoms. Research has shown that screening men and women for bowel cancer using FOB Test can reduce the mortality rate from bowel cancer by 16% in those invited for screening. The aim is to detect bowel cancer at an early stage when there is a better chance of a person being successfully treated and cured.
Those eligible for screening will receive a kit for use in the privacy of their home. The FOB test kit is then analysed to detect traces of blood that may not be visible to the naked eye. The FOB test is NOT a diagnostic test for cancer; however, the result will indicate whether further investigation is required.
Around 98% will receive a normal result and will be invited to participate again in a further 2 years’ time, if still eligible. Around 2 in 100 people will receive an abnormal/positive result. They will be referred to see the Specialist Bowel Screening Nurse to discuss and arrange a Colonoscopy. After having a positive/abnormal FOB Test and after a colonoscopy
- Approx 6 in 10 people will have a normal result
- Approx 3 in 10 people will be found to have a polyp
- Approx 1 in 10 people will have cancer detected
Bowel Scope Screening (55 years)
Bowel scope screening involves a flexible sigmoidoscopy. The aim is to find any small growths called ‘polyps’, which may develop into bowel cancer if left untreated. Bowel scope screening is an addition to the existing NHS Bowel Cancer Screening Programme that starts at age 60.
Colonoscopy
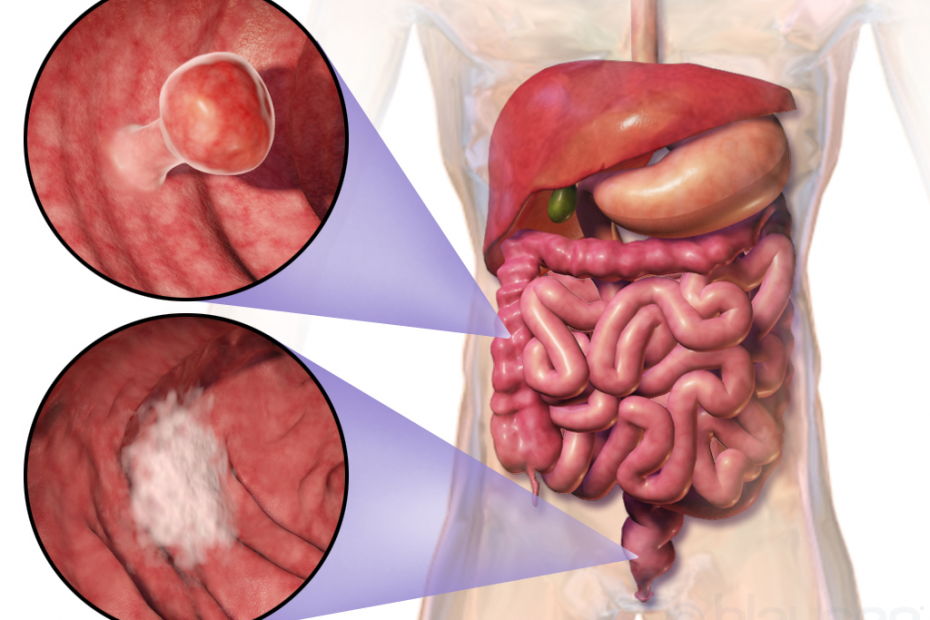
Colonoscopy is a test which allows the endoscopist to directly examine the lining of the large intestine (the colon). Diagnostic colonoscopy is recommended for persistent change in bowel habit, occult or frank blood in the stool, unexplained anaemia and as a screening test for colon cancer. In order to do the test a colonoscope is carefully passed through the anus into the rectum and advanced through the intestine. The colonoscopy is a long flexible tube, about the thickness of your index finger, with a bright light and video camera at its tip. The video camera on the colonoscope transmits images of the inside of the colon to a monitor, allowing the endoscopist to examine the lining of the colon for any disease or abnormalities.
What else may be done during the procedure?
During the colonoscopy a biopsy (a sample of the lining of the bowel for closer examination under the microscope) may be taken using tiny biopsy forceps passed through the colonoscope. This is a painless procedure.
It is also possible to remove polyps during a colonoscopy. Polyps are abnormal projections or growths of tissue from the lining of the bowel, rather like a wart, and certain types of bowel polyps may be at risk of developing into cancer if left. If polyps are found the endoscopist may decide to remove them via polypectomy during the procedure; again this is a painless procedure. Occasionally it may be necessary to return for a repeat colonoscopy in order to treat large or difficult to remove polyps.
Bowel preparation
To allow a clear view, the colon must be clean and completely empty of waste material. It is important to take all of the laxatives prescribed and considerably increase your intake of clear fluids on the day before the examination, which will help clean the bowel. Please also follow the dietary instructions for the few days preceding the test, as this will also help to ensure the bowel is clean for the test.
When you come to the department, a member of staff will explain the test to you and ask you to sign a consent form. This is to ensure that you understand the test and any potential complications that may occur. Please tell the doctor of nurse if you have had any allergies or bad reactions to drugs or other tests in the past. They will also want to know about any previous endoscopy you have had, or any other medical conditions which you may suffer from and details of medication which you may be taking.
During the procedure
You will be placed in a comfortable position on your left side, and may be given medication by injection through a vein to make you sleepy and relaxed. The endoscopist will then pass the colonoscope into the rectum, and advance it through the colon. Colonoscopy is not usually painful. You may experience some abdominal cramping and pressure from the air which is introduced into your bowel; this is normal and will pass quickly. You may also be asked to change position during the examination, and will be assisted by a nurse. The examination usually takes anywhere from 15-60 minutes.
After the procedure
You will be left to rest in the recovery area for up to 1 hour, until the main effects of any medication wear off. A responsible adult must be available to escort you home as the sedation impairs your reflexes and judgement. For the remainder of the day you should not drive a vehicle, operate machinery or make important decisions. We suggest that you rest quietly.
When will I know the results?
In most cases a member of staff will be able to tell you the results of the test as soon as you are awake and you will give a copy of the endoscopy report to take home. However, if a biopsy sample or polyp was removed for microscopic examination these results may take up to two weeks to process.
What to expect after a Colonoscopy?
You may resume your normal daily activities the day after the examination.
The doctor or nurse will have told you before being discharged if you had biopsies taken or polyps removed. If this was the case, you may notice traces of blood coming from your back passage. If bleeding persists, becomes more severe or the abdominal pain becomes worse, you should contact the physician.
Food and drink
Alcohol in combination with any sedation you may have received is likely to make you much more sleepy than usual. Normal food can be taken after the examination, though you may prefer light meals on the day of the examination.
Medications
You may resume normal medications immediately after your colonoscopy but if a polyp was removed we may advise against taking certain blood-thinning or anti-inflammatory drugs for a defined period. Please ask if you are not sure that a medication will be safe. You may take stool softeners and bran but do not take strong laxatives.

Bowel actions
Your colon has been completely emptied and you should not expect necessarily to start to have normal bowel function for two to three days. Bowel actions after that should rapidly return to normal.
Things to report to your doctor
- Severe pain or vomiting
- Passage or vomiting of blood
- Temperature greater than 38 degrees
- Redness, tenderness and swelling at the site of the intravenous injection that persists